History
OUR HISTORY
Healthcare is one of the largest industries in the U.S., with 38 of 50 states having healthcare as their top employer, and U.S. spending on healthcare is $5 trillion. Yet health outcomes, affordability and accessibility are declining. In New York City – the wealthiest city in the world – worsening working conditions for healthcare workers means that fewer poor and working people are able to get the care they need. Despite New York having some of the top medical facilities in the country, the majority of New Yorkers live in “medical deserts” with little to no primary care services in their neighborhoods.
Doctors, dentists, nurses, physician assistants and workers across all specialties are facing short staffing, high costs of practicing and shrinking reimbursements. Healthcare professionals are forced by insurance companies to treat their patients as products on a conveyor belt, getting patients in and out the door as fast as possible. The majority of health professionals now work in large group practices. Many of them are now owned by private equity, whose primary objective is to increase profit, not to provide care. Diabetes, hypertension and infant mortality – mostly preventable – all continue to increase across the nation, and treatable-but-untreated conditions languish as workers cannot afford the resources to achieve and maintain good health.
The rise of the insurance industry, Health Maintenance Organizations (HMOs) and “managed care” within healthcare have also contributed to worse health outcomes for working people. Since the U.S. manufacturing industry began to decline throughout the 1960s and 1970s, more employers have shifted to working with HMOs to cut costs on healthcare benefits for employees. But as HMOs continue to gain monopoly control over what healthcare is available, in what quantities, and to whom, more U.S. residents are facing the contradiction of having health insurance without having real health coverage. Federal reforms like Medicaid and Medicare were undercut by state-wide waivers to the Social Security Act’s Title XIX and Title XX, while the Affordable Care Act fell far short of its promise of “universal healthcare.” What benefits were available are threatened as federal public health budgets have decreased since the 2008 Great Recession.
Coalition of Concerned Medical Professionals (CCMP) has spent over five decades organizing healthcare professionals, students, clergy and concerned residents to fight for comprehensive healthcare and build our preventive medical benefit program. What you will find below is a brief overview of CCMP’s history in the New York Metropolitan area. To get the whole story, and help make history, come into CCMP’s office and participate in the effort to make healthcare a human right.
1973
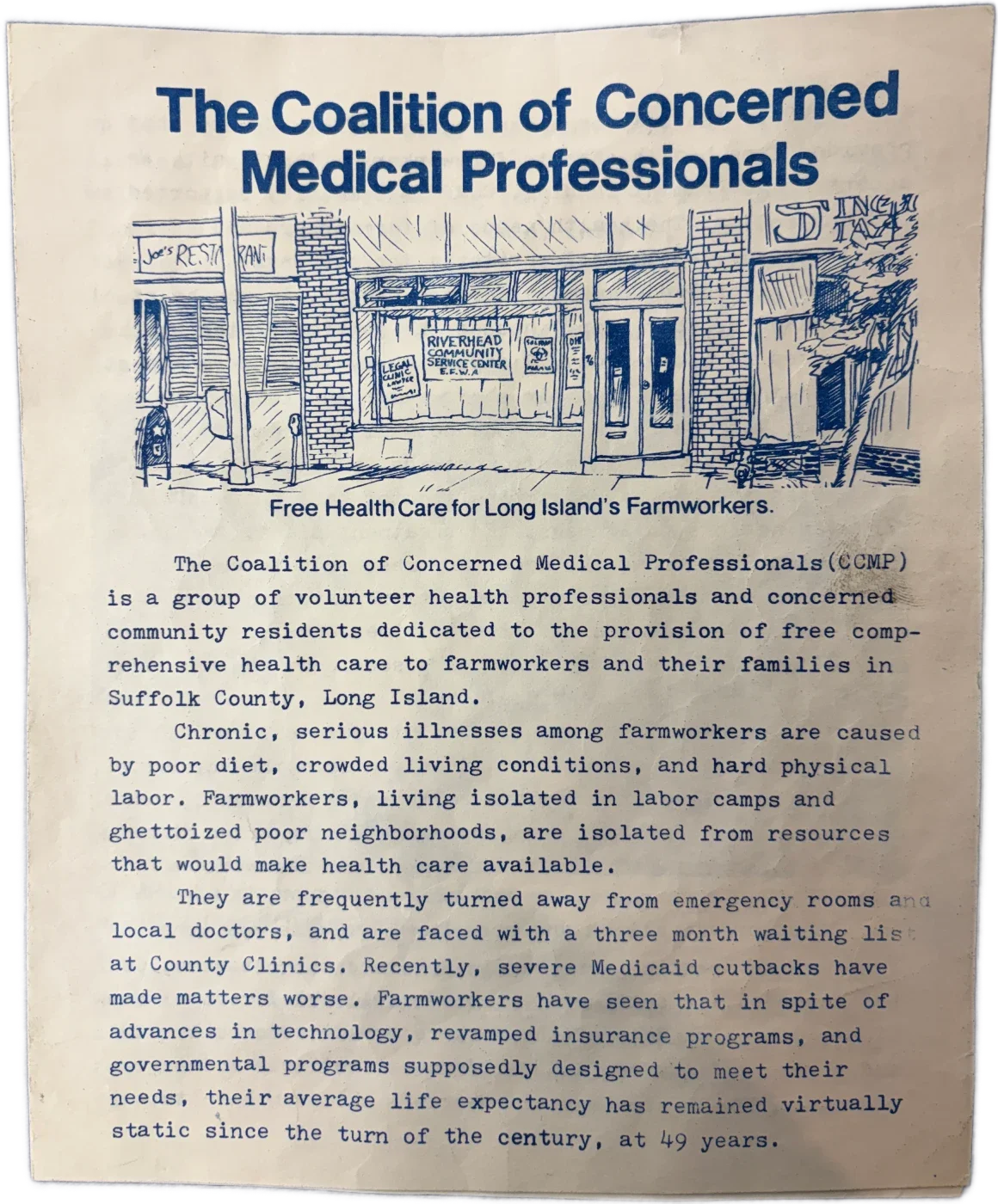
CCMP was established in Riverhead, New York in 1973 in response to growing organizing throughout the farm labor camps in Suffolk County on Long Island. CCMP formed, having grown out of the preventive medical benefit program of Eastern Farm Workers Association (EFWA), which had been founded the year prior in 1972. In response to a total abandonment of the farm workers of Suffolk by both county and state government officials, EFWA organized doctors, an order of nursing nuns, medical students from SUNY Stony Brook’s Medical Center and others to go out to the farm labor camps to do screenings of growing diseases and provide preventive medical services free of charge.
These health professionals, students and concerned community residents uncovered a host of treatable-but-untreated conditions among the workers such as diabetes, hypertension and seizure disorders caused primarily by pesticide exposure. The health professionals agreed that the conditions of the farm workers called for permanent organization, and founded CCMP in 1973.
1974
Within a year of CCMP’s founding, CCMP member health professionals and volunteer organizers founded the Occupational Health Project (OHP) to address farm workers’ exposure to pesticides. Temik, the major pesticide used for potatoes at the time, was causing severe seizures among many Suffolk farm workers. However, when farm worker patients showed up in emergency rooms, they would often be sent home diagnosed as epileptics or disregarded as “probable alcoholics.” CCMP health professional members and volunteer researchers conducted a study of dead animals littering the farms and secured samples of the pesticide. They used the data to release a report which conclusively identified Temik as the cause of the farm workers’ illness. This resulted in better medical treatment for the farm workers. Temik was finally banned in Suffolk County in 1980.
OHP later won the first workers’ compensation cases for Puerto Rican landscape nursery workers. The workers were frequently injured on the job, and if they had to leave the job early due to injury or disability, they were sent home without any pay. Prior to OHP, it was unprecedented for these workers to receive any compensation for their injuries.
1975
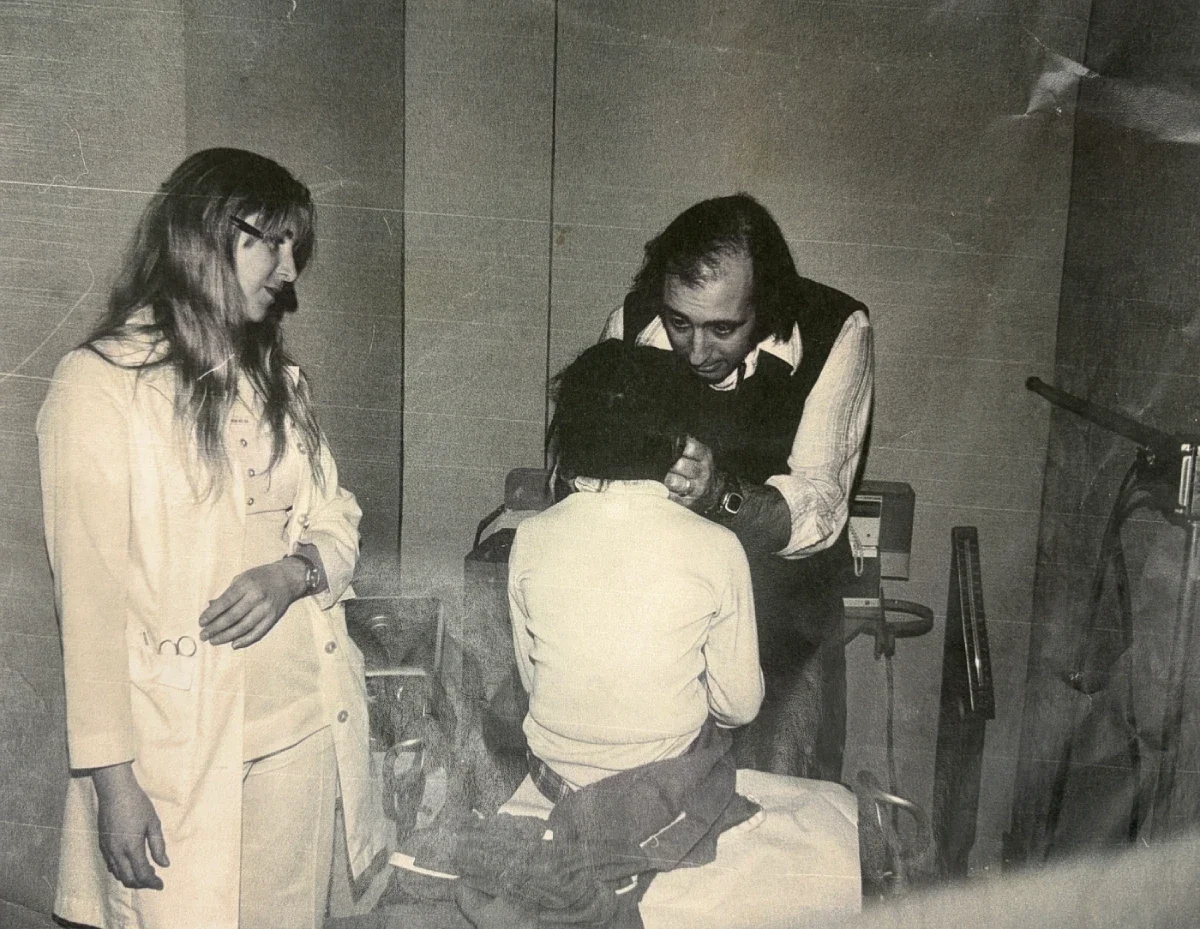
Dr. Leo Galland, then an attending physician and professor at SUNY Stony Brook, joined as CCMP’s first medical director in 1975 helping to build CCMP’s preventive medical benefit and strengthen CCMP’s ties with Stony Brook faculty and students.
1979 - 1980s
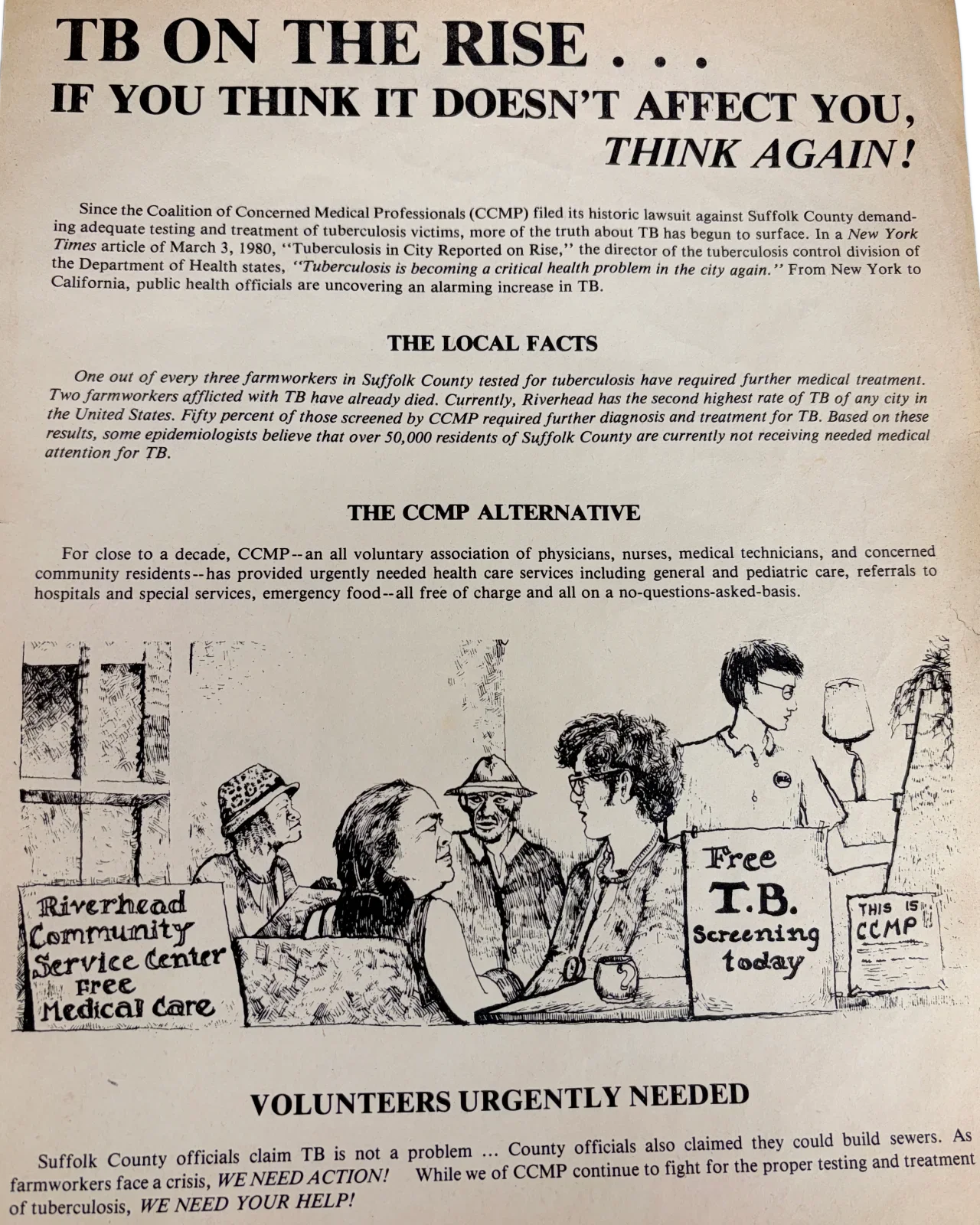
In 1979, CCMP member doctors found that seven out of nine farm workers seen at CCMP general medical sessions were testing positive for tuberculosis. CCMP organizers then approached the Suffolk County Department of Health to ask for treatment for the affected farm workers, and to ask what their plan was to stop the spread of tuberculosis. When county officials refused to assist, CCMP members and volunteers organized what resources they could to test and treat the workers while also publicizing the county’s failure to act. CCMP galvanized broader community support throughout a series of legal battles and began to build the base of support necessary to establish an office in the five boroughs.
1985
Dr. Gerald Deas
In Memoriam 1931 to 2026
During the course of CCMP’s campaign to get care for farm workers with tuberculosis, Dr. Gerald Deas joined the fight. After signing up at an information table in front of a market in Suffolk County in 1985, he subsequently became CCMP’s Medical Director for over 20 years and helped to grow our base of support and volunteer participation of doctors throughout the New York area. Dr. Deas was an acclaimed physician, and was the first Black class president when he graduated from SUNY Downstate College of Medicine. He was also the first Black medical columnist for the New York Daily News, a host of a weekly radio show on WLIF, and a leading public health advocate on several campaigns to improve the health of low-paid workers and communities of color in New York. He would regularly promote CCMP through his radio shows and through his TV show through Downstate. He not only led general medical sessions, medical education and information sessions and other tactics with CCMP, but also played a pivotal role in growing CCMP’s relationships with other healthcare institutions and practitioners.
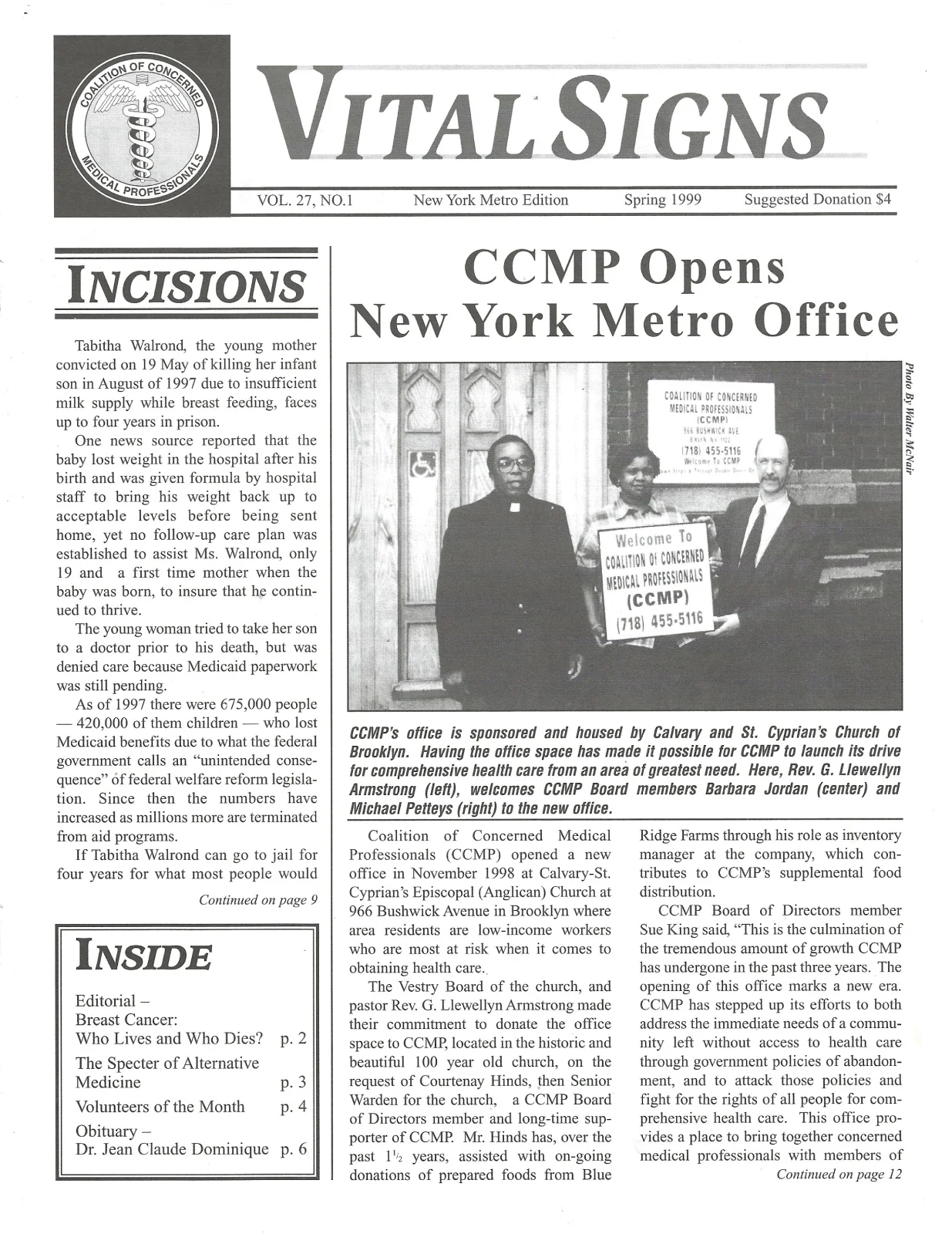
1998
In November 1998, CCMP opened our first office in the New York metro area at Calvary & St. Cyprian’s Episcopal Church at 966 Bushwick Avenue in Brooklyn. The church committed to donate office space to CCMP upon the request of Courtenay Hinds, then the senior warden for the church, who is a CCMP Board of Directors member and long-time supporter. The church is on the border of the Bushwick and Bed-Stuy neighborhoods, then one of the poorest areas in Brooklyn – a very central location for our benefit recipients. CCMP operated out of Calvary & St. Cyprian’s for two years while continuing to expand our programs. The church remains an ardent supporter and host of many CCMP community canvasses, special events and other activities throughout the year.
2006
In 2006, Dr. Michael Feldman of East Coast Endodontics began donating what would become annual root canal sessions for CCMP benefit recipients. Dr. Feldman, a member of CCMP’s Board of Directors, along with his staff donate as many as 20 root canals in a day. Root canals are one of the most difficult and expensive procedures to get covered by insurance; New York Medicaid policy specifically states they will only pay for root canals if extracting the tooth is “medically inadvisable.” However, root canals preserve a patient’s natural teeth and can maintain better oral health for decades. CCMP always needs more dentists, dental specialists and dental labs to help expand this always growing portion of our benefit program.
2011
After years of moving through donated and rented spaces, CCMP obtained a permanent base of operations to ensure stability into the future. CCMP Board of Directors member and podiatrist Dr. Lawrence Cohen’s former office became CCMP’s permanent headquarters in Canarsie, Brooklyn. With the help of local unions, contractors, building supply companies and others, CCMP has continually improved the working space of our office.
2012
After just a year of occupying our new Canarsie office, New York City was hit by Hurricane Sandy. A massive problem became apparent once the flood waters receded: mold. CCMP formed a Disaster Relief and Health Impact Committee. We canvassed door-to-door, documenting the problems being experienced by residents. Many were not getting assistance from their insurance company because they had no flood insurance, and the government agencies would not help because they did not consider them to be “flood” victims. They claimed the sewer system had backed up, causing the damage – not rising flood waters. In light of the city shirking responsibility, CCMP’s Board member and air quality specialist Pierre Cajuste partnered with fellow Board member Dr. David Scott to lead a medical education and information session on mold abatement, hosted by local business supporter Juana Sosa at Truly Dominican Hair Salon. Volunteers also organized donated sheetrock to replace walls for those who had no other means to repair the water damage.
2020-2021
During the COVID-19 pandemic, not only did CCMP never shut down our operations for a single day, but CCMP volunteer organizers went on the offensive, immediately adopted necessary public health safety protocols and began organizing our volunteers to canvass low-income neighborhoods and establish an Emergency Food Benefit to provide donated non-perishables for those suffering in the pandemic. CCMP members also conducted a series of medical education and information sessions to inform the community about COVID-19, vaccines and much more.
2024 - 2025
In 2024, CCMP launched a Save Our Hospitals campaign in response to New York State threatening to close SUNY Downstate Medical Center. Downstate is an acclaimed facility, hosting the only kidney transplant center in Brooklyn along with several other specialist departments, and is the fourth-largest employer in the borough. CCMP partnered with members from United University Professions (UUP) and Public Employees Federation (PEF), as well as congregants of Lenox Road Baptist Church, to organize speaking engagements, attend rallies and public hearings, and run a postcard campaign demanding that the governor and state government not only use the $10 billion that New York City and State gives away in tax breaks to the top 1% of corporations each year to fund Downstate, but to end the state’s pattern of hospital closures and chronic understaffing. CCMP mailed over 3,000 postcards. In 2025, Governor Kathy Hochul announced that the hospital would remain open and that the state would allocate $1.1 billion in funding for capital improvements.
Join with CCMP to write the next chapter!